Abstract
Introduction
Disparities in clinical trial enrollment have the potential to bias findings, limit generalizability, misdirect drug development, and reduce equitable access to novel therapy. Given the unique care delivery and clinical trial patterns of acute leukemia (AML), barriers to trial enrollment for underrepresented groups at the Comprehensive Cancer Centers (CCCs), where patients are often treated, may be distinct. Characterization of these barriers has been limited, preventing the development of interventions to overcome this disparity for AML.
Methods
We conducted an exploratory qualitative project to characterize barriers to trial enrollment and facilitators to overcome them through a series of focus groups and individual interviews. Participants were persons with AML who identified from one or more underrepresented groups and AML physicians, nurse practitioners, and physician assistants at three Dana-Farber/Harvard Cancer Center hospitals. A moderator guide was developed based on literature review and iteratively revised by study investigators. The questions enabled an open-ended multi-level (patient, provider, trial, institution, societal) exploration of five main domains, including familiarity and experience with clinical trials, factors influencing participation, participant concerns and enrollment supports, and facilitators to address enrollment barriers and disparities. Focus groups and interviews occurred through video conference or phone and were audio recorded and professionally transcribed. The interdisciplinary research team conducted a multi-step thematic analysis guided by framework analysis, and included prefigured and emergent codes. The team-based analysis synthesized data within and across participant types and focused on the identification of key patterns and prevalent themes related to barriers to clinical trial enrollment. Coding and analysis were assisted by NVivo 12 software. Results presented below highlight barriers that were considered relevant to the unique care delivery patterns of AML and clinically significant.
Results
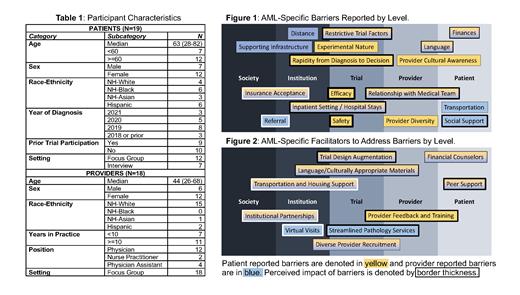
37 participants (19 patients; 18 providers) were recruited to focus groups (30) or interviews (7) between 5/6-6/28/2021. Participant characteristics are shown in Table 1. Patient participants were generally familiar with clinical trials. Despite limited explicit expression of enrollment hesitancy, both patients and providers noted multiple potential barriers to clinical trial enrollment specific to AML, including the rapidity from diagnosis to treatment; the inpatient setting of therapy; a lack of knowledge regarding incidence and enrollment demographics and their differences; restrictive trial design factors (e.g., hospital stays, mutation specificity); and concerns over the appropriateness and efficacy of a given trial relative to individual disease risk. Key enrollment barriers reported by participants are shown in Figure 1. Participant-identified facilitators to address these barriers are shown in Figure 2. Facilitators to overcome barriers specific to AML that were considered potentially impactful included: peri-enrollment peer support for patients, continuance of telehealth visits during trial participation, feedback and training to increase provider awareness and understanding of disparities and diverse communities, trial design augmentation to minimize restrictive barriers (centralized laboratory draws, multiple hospitalizations, white blood cell count and organ function criteria) and increase inclusivity (multiple language and culturally competent consent), and bolstering inter-institutional AML program partnerships to increase diverse patient referral.
Conclusions
Stakeholder-reported barriers to diverse AML clinical trial enrollment at CCCs include multiple disease-specific characteristics that reflect the unique care pattern of AML, such as concerns about restrictive trial design characteristics, the need to be inpatient, and the requirement to make decisions quickly after diagnosis. Several barriers and potential interventions at each level were considered impactful by both providers and patients. These formative data suggest a novel multi-level approach for overcoming AML enrollment disparities at CCCs is needed.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal